Ontario Stroke Report 2019/20 Overview
Ontario’s Annual Stroke Report provides an overview of stroke system performance in the province. The eleven (11) provincial stroke networks use this report to enable system planning and decision making, reflecting best practice, leading to system improvements, and ultimately better outcomes for patients and families with stroke.
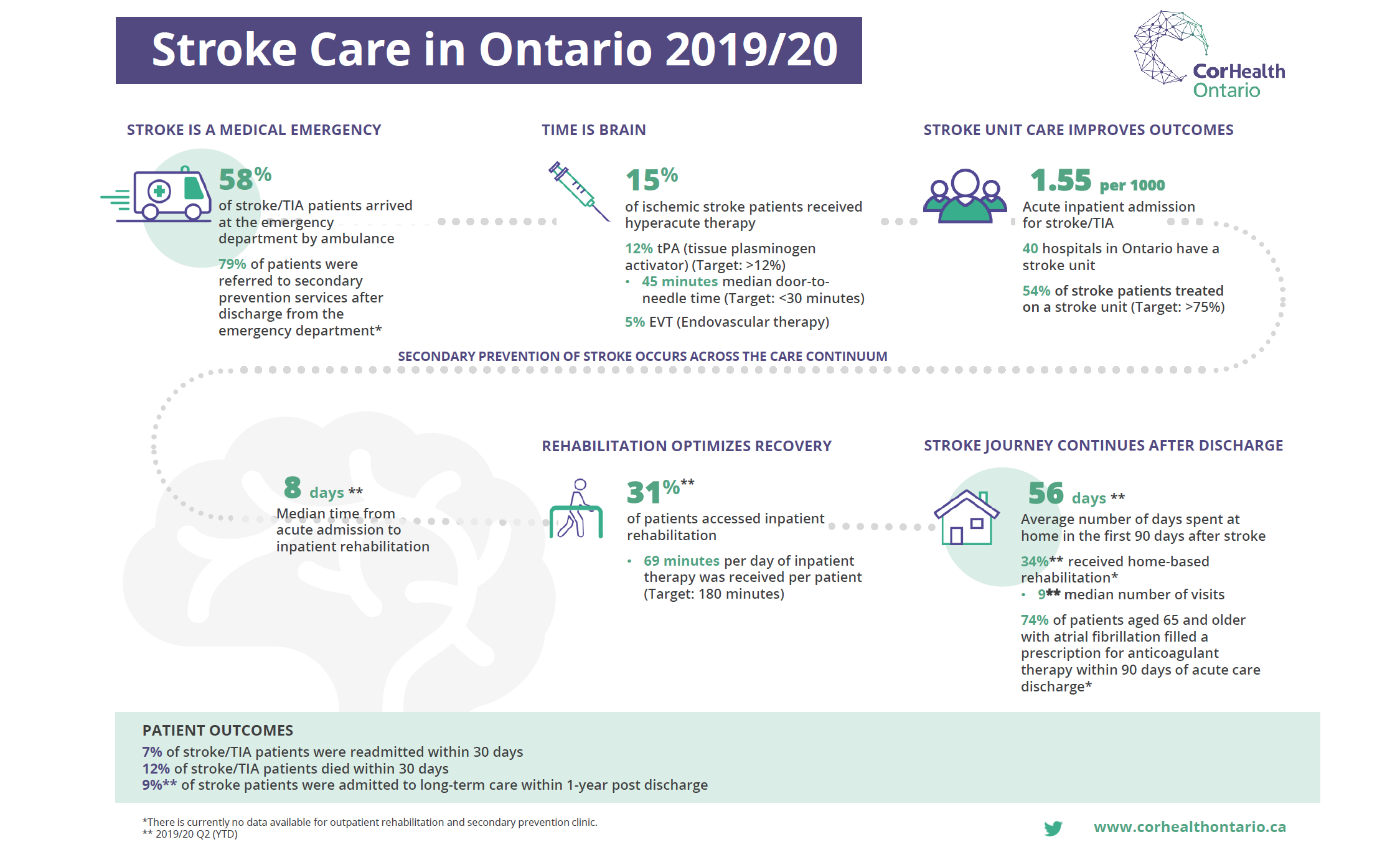
In the 2019/20 Ontario Stroke Report, a few key highlights from the report show that stroke patients’ access to hyperacute care has grown in the past few years. Most of this growth is attributed to the introduction and steady growth in access to endovascular therapy (EVT). The goal of early acute treatment is to restore blood flow to the brain and to preserve brain tissue. Median door to needle time for patients who received tissue plasminogen activator (tPA) decreased from 47 minutes (2018/19) to 45 minutes (2019/20) equating to approximately 4 million neurons saved per patient.1 It is important that work continues to reduce door to needle times towards a target of 30 minutes, to optimize the effectiveness of this treatment in reducing the impact of stroke.2
An area for improvement is in access to stroke unit care. Patients who receive stroke unit care are more likely to survive, return home and regain independence compared to patients who receive generalized care.1 In 2019/20, only 54% of Ontario’s stroke patients received care on a stroke unit, and there is a wide range across the province in the proportion of patients that received care on a stroke unit. Access to stroke unit care has also been found to influence access to other stroke best practices such as timely and appropriate stroke rehabilitation and applicable diagnostics such as carotid imaging. Further system planning is required to optimize the benefits of stroke unit care and meet the target of 75% access.2
Another area for improvement, is in the rehabilitation sector. Stroke rehabilitation is a critical component of recovery, helping patients to regain lost skills, relearn tasks and regain independence. Stroke rehabilitation is an essential part of the care continuum, requiring a systems approach to optimize availability of services, ensure capacity and facilitate access to the right level of care based on patient needs. This would include consideration of early supported discharge, inpatient, and community-based programming (home based and outpatient). Many patients did not receive the required rehabilitation therapy (intensity), receiving 69 minutes per day of direct therapy, well under the 180 minutes per day of direct therapy that is recommended in the Canadian Stroke Best Practices and adopted by Health Quality Ontario and the Ministry of Health and Long-Term Care, Quality Based Procedures Clinical Handbook for Stroke. In 2019/20, approximately 50% of stroke patients accessed post-acute rehabilitation (inpatient and/or home-based). Additional data is required to fully understand system capacity and access to post-acute services. Currently, there is no standardized provincial system to capture the number of stroke patients that access outpatient rehabilitation services. Furthermore, home-based rehabilitation provided by hospitals is not captured in the homecare database (HCD).
The annual Stroke Report acts as a foundation for knowledge exchange and quality improvement at a system and organizational level. CorHealth Ontario will continue to collaborate with Ontario’s 11 Regional Stroke Networks to align operating plans, knowledge translation approaches and implementation strategies to continue to advance best practice stroke care across the province.
2019/20 Stroke Care in Ontario Infographic
To capture key highlights from the report, CorHealth Ontario in collaboration with key stakeholders have developed the Ontario 2019/20 Stroke Care in Ontario infographic. Please click here to view the infographic.
In addition to the infographic, the Stroke Regional Directors and District Stroke Coordinators, have been provided with a comprehensive report that captures additional performance indicators for stakeholder engagement and quality improvement.
If you have any questions, please contact us at oh-corh_service@ontariohealth.ca
1Boulanger, J., Lindsay, M., Gubitz, G., Smith, E., Stotts, G., Foley, N., … Butcher, K. (2018). Canadian Stroke Best Practice Recommendations for Acute Stroke Management: Prehospital, Emergency Department, and Acute Inpatient Stroke Care, 6th Edition, Update 2018. International Journal of Stroke, 13(9), 949–984. https://doi.org/10.1177/1747493018786616
2Heart & Stroke Foundation. Canadian Stroke Best Practices Stroke Quality Advisory Committee. Quality of Stroke Care in Canada. Update 2016 Final (R12). Accessed April 15, 2021 at https://www.strokebestpractices.ca/-/media/1-stroke-best-practices/quality/english/2016strokekeyindicators.ashx
Data Disclaimer:
This study made use of de-sensitized data from the ICES data repository, which is managed by the Institute for Clinical Evaluative Sciences with support from its funders and partners: Canada's Strategy for Patient-Oriented Research (SPOR), the Ontario SPOR Support Unit, the Canadian Institutes of Health Research (CIHR) and the Government of Ontario. The opinions, results and conclusions reported are those of CorHealth Ontario. No endorsement by ICES or any of its funders or partners is intended or should be inferred.
Parts of this material are based on data and/or other information compiled and provided by CIHI. However, the analyses, conclusions, opinions, and statements expressed in the material are those of the author(s), and not necessarily those of CIHI.